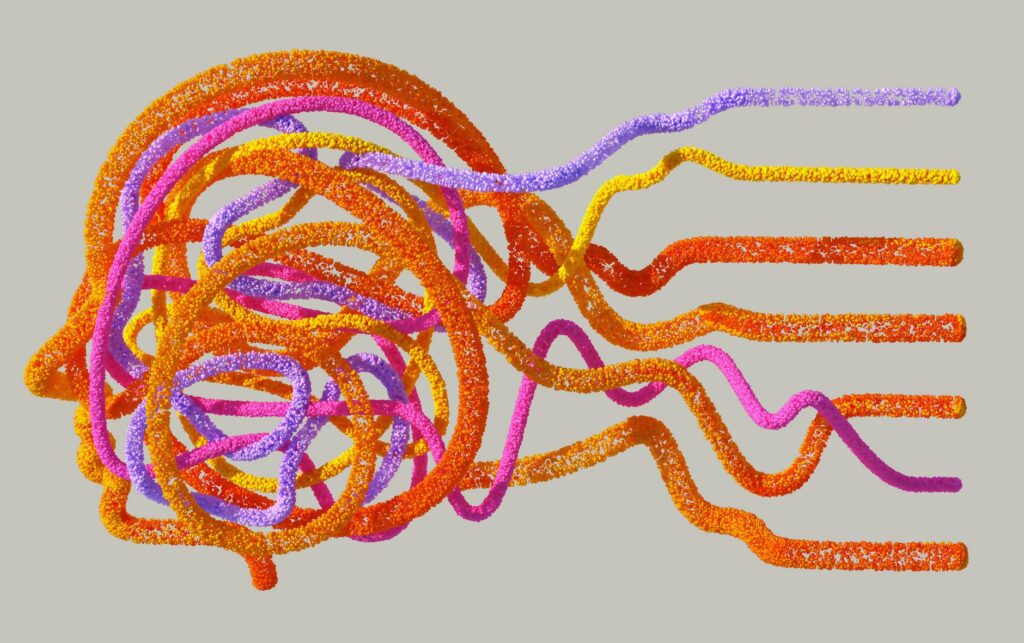
Scientists have taken a major step toward decoding the complex brain mechanisms that underlie schizophrenia and bipolar disorder. A collaborative study, recently reported on ScienceTechDaily, combined high‑resolution brain imaging with large‑scale genetic analysis to pinpoint overlapping and distinct neural circuits affected in both conditions. The findings suggest that disruptions in specific pathways—particularly those linking the prefrontal cortex, hippocampus, and thalamus—may drive the hallmark symptoms of psychosis, mood swings, and cognitive deficits. This breakthrough not only deepens scientific understanding but also opens new avenues for targeted diagnostics and therapies.
Mapping the brain’s wiring
Researchers employed diffusion tensor imaging (DTI) and functional MRI to trace white‑matter connections across the brains of over 3,000 participants, including patients with schizophrenia, bipolar disorder, and healthy controls. The analysis revealed reduced integrity in the fronto‑striatal and cortico‑thalamic pathways, both of which are critical for executive function and emotional regulation. Notably, these disruptions were present in both disorders, indicating a shared neurobiological substrate.
Genetic signals meet neural circuits
Parallel genome‑wide association studies (GWAS) identified several risk genes—such as GRIN2A, NRG1, and CACNA1C—that are highly expressed in the affected brain regions. By overlaying the genetic risk maps onto the imaging data, the team demonstrated that variants in these genes correlate with the degree of white‑matter degradation, suggesting a direct link between genetic susceptibility and structural brain changes.
Implications for diagnosis and treatment
The convergence of imaging and genetics offers a potential biomarker panel that could differentiate between schizophrenia and bipolar disorder with greater precision than symptom‑based assessments alone. Clinicians may eventually use a combination of DTI metrics and a polygenic risk score to tailor interventions—ranging from antipsychotic medication to neuromodulation techniques—based on an individual’s neural profile.
Future directions and ethical considerations
While the study marks a milestone, researchers caution that brain circuitry is only one piece of a multifactorial puzzle that includes environment, lifestyle, and psychosocial factors. Ongoing longitudinal studies aim to track how these neural signatures evolve over the course of illness and treatment. Moreover, the prospect of predictive testing raises ethical questions about privacy, stigma, and the responsible use of genetic‑neuroimaging data.
| Brain region | Observed change | Associated risk genes |
|---|---|---|
| Prefrontal cortex | Reduced fractional anisotropy | GRIN2A, CACNA1C |
| Hippocampus | Volume loss | NRG1, C4A |
| Thalamus | Disrupted connectivity | GRIN2A, CACNA1C |
| Striatum | Altered dopamine signaling pathways | DRD2, ANK3 |
In summary, the integration of advanced neuroimaging with large‑scale genetic data has illuminated a shared neural framework underlying schizophrenia and bipolar disorder, while also highlighting disorder‑specific variations. These insights pave the way for more accurate diagnostics, personalized treatment strategies, and a deeper appreciation of the brain‑gene interplay that drives mental illness. As research progresses, balancing scientific innovation with ethical stewardship will be essential to ensure that these breakthroughs translate into real‑world benefits for patients.
Image by: Google DeepMind
https://www.pexels.com/@googledeepmind